Adopt an employee-focused approach by using Certilytics library of 1,000+ clinical, financial and behavioral predictive risk scores to identify future risks and opportunity to improve outcomes and lower costs by employee.
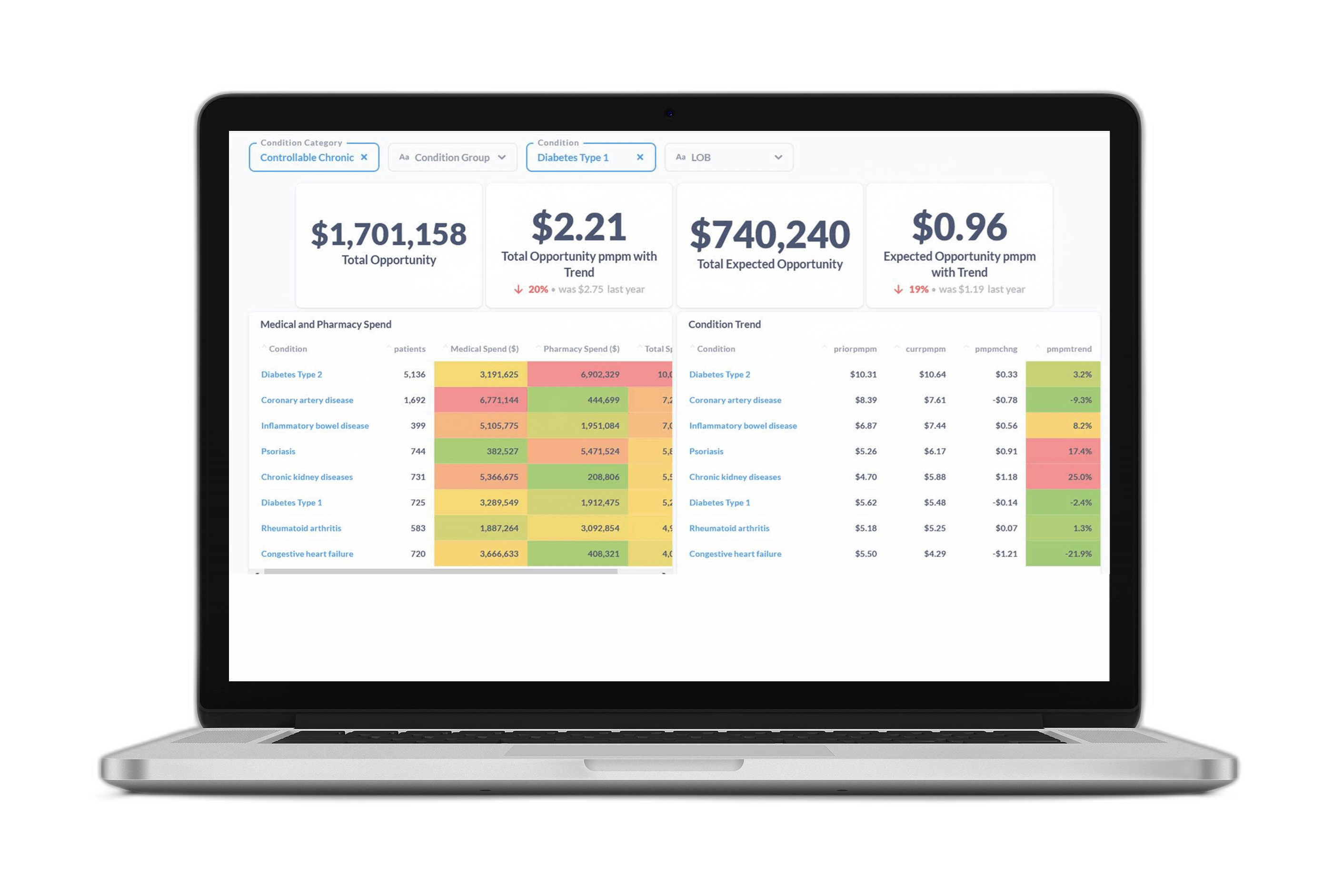
Highlight the most common health conditions impacting employee well-being and forecast potential disease onset and their associated costs with the Opportunity Analyzer.
Create a benefit plan tailored to the specific healthcare needs and risks of your workforce, as well as make recommendations for programs and strategies with the greatest opportunity for lowering costs.
Identify how likely someone is to engage in a program, with Certilytics’ Outreach Optimizer so you can be confident your programs are reaching those employees who are most likely to modify their behavior and improve their health.