AvMed, one of Florida’s oldest and largest not-for-profit health plans, and Certilytics, Inc., a healthcare predictive analytics company founded in 2014, are expanding their partnership to provide employer groups with comprehensive, AI-powered reporting to help improve employee wellness and manage costs.
The partnership between AvMed and Certilytics will equip employer groups with value-focused analytics that enable effective member outreach, provider engagement strategies, specialty drug management, and more.
“We are excited to grow our relationship with Certilytics and look forward to leveraging their cutting edge data analytics tools to better serve our members, employer groups and provider partners,” said Eric Johnson, senior vice president, chief actuary and chief information officer for AvMed. “We are eager to partner with Certilytics to optimize our use of data to improve outcomes and increase member satisfaction,” added Johnson.
“We’re thrilled to be expanding our partnership with AvMed, which has shown a strong commitment to being at the forefront of using advanced predictive analytics to inform effective member outreach and engagement strategies,” said Jessica Kinnick, senior vice president for client deployment and adoption at Certilytics. “We look forward to continuing to support AvMed in providing a market-leading reporting package for employer groups.”
The expanded partnership will include:
- The use of Certilytics’ CORE Pathways clinical episode grouper and Forecasts member-level risk stratification tool to support effective clinical outreach informed by predictive opportunity and propensity modeling around member engagement
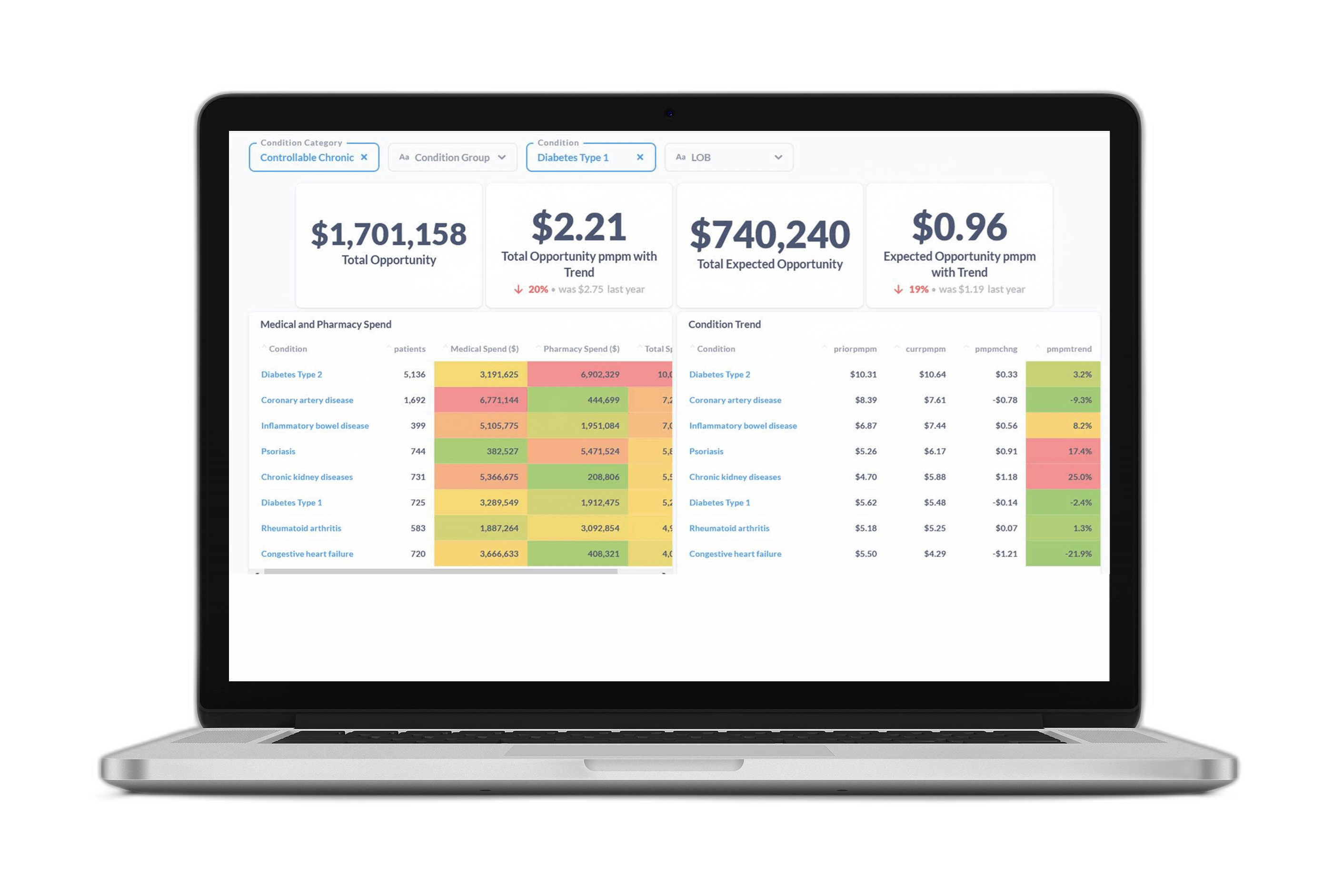
- The Opportunity Analysis population-level reporting package to support resourcing decisions around health management strategies aimed at closing gaps in care, redirecting members with high-cost utilization patterns, and intervening earlier with those at risk for chronic conditions
- Dashboards and reporting to support provider engagement strategies, earlier identification of potential high cost claimants, and management of specialty drugs as part of an employer group reporting package
- Development of a suite of custom predictive models, including a model to support better management of patients receiving palliative care
- Use of Certilytics’ Fusion business intelligence tool for deeper insights into cost and utilization trends